Georgia’s Healthcare Reform
Sector research is one of the key directions of Galt & Taggart Research. We currently provide coverage of Energy, Healthcare, Tourism, Agriculture, Real Estate, and Wine sectors in Georgia. Here we provide an overview of Georgia’s healthcare reform, while in the next article we will discuss the sector’s current state. The full report on Georgia’s healthcare sector can be found on Galt & Taggart’s website - gt.ge
Over the last 15 years, Georgia’s healthcare system has undergone effective reforms, which have improved health indicators and narrowed the gap between Georgian and European standards. However, the road to the current universal healthcare (UHC) model, with an improved structure and legal framework, was long and winding.
After Georgia regained independence in 1991, private spending became the major source of healthcare financing, as annual public per capita funding slumped to US$ 0.5 from US$ 149 in 1990. Following the Soviet Union’s dissolution, Georgia, like other former Soviet states, could no longer afford a Soviet-style, cradle-to-grave healthcare system. In 1994, a plan was designed to restructure the healthcare system, defining the legal framework and the financing scheme of the sector. In addition, efforts were made to soften the reliance on the Soviet-style Semashko model. To that end, in 1995, the state declared for the first time that healthcare would no longer be free of charge.
A new direction was set in 2003, aimed at liberalizing healthcare policy and boosting competitiveness through major changes, including but not limited to easing regulations and letting private companies enter the market. Medical services have been exempt from most major taxes since 1997. In 2005, the number of required general healthcare licenses was cut from 302 to 42, as the number of overall business activities subject to licenses and permits was reduced by 84%. In March 2006, the Ministry of Labor, Health, and Social Affairs of Georgia (MoLHSA) established guidelines for care, against which patient complaints would be examined. The old Soviet state-run centralized Semashko healthcare model, which had been gradually softened, was finally shut down in 2007, as Georgia moved to an insurance-based healthcare model.
Under the insurance-based healthcare model, the government started to purchase private health insurance packages for the neediest (0.75mn people or 21.3% of the population) in 2007 and expanded coverage to Internally Displaced Persons (IDPs) and beneficiaries of child care institutions in 2008. According to the model, public funds went to private insurers, who delivered care to eligible citizens mostly through their own, privately run hospitals. This change marked a makeover of public healthcare provision, as the model handed healthcare delivery over to private companies. The second stage of public insurance came in September 2012, with the expansion of state coverage to children aged 0-5, pensioners, students, and disabled individuals (an additional 0.9mn people or 19.8% of the population, for a total of 1.8mn people or 41.1% of the population). After the 2nd stage of public insurance coverage expansion, the healthcare model came closer to a UHC system.
In 2007, the government also initiated the Hospital Development Master Plan, with the goal of privatizing hospital infrastructure within 3 years. The reform was designed to reduce the number of hospital beds from 14,600 in 2007 to 7,800 in 2010 (of which 1,860 beds would remain in state ownership). Due to a lack of expertise from investors, the armed conflict with Russia in August 2008, and the ensuing economic recession, privatization efforts stalled and almost none of the privatized assets were duly renovated. In 2010, the government adjusted the plan and combined hospital operation and the provision of health insurance. The country (excluding Tbilisi) was divided into 26 healthcare districts. Insurance firms were invited to participate in tenders to provide coverage to eligible citizens. The winning insurers were obligated to build or renovate and operate hospitals in their respective regions by the end of 2011 or 2012. In that respect, as of end-2013, up to 150 new hospitals had been built and opened for operation. The new hospital owners also invested in renovating facilities, equipping them with up-to-date equipment and improving human resources.
In 2013, in order to improve financial accessibility of healthcare services, the Georgian government introduced a UHC system for the entire population. The UHC reform consolidated government-funded (general coverage) healthcare programs under the UHC umbrella, including the ones administered by private insurance companies, with any citizen eligible for coverage. Implementation started in March 2013. The introduction of an extended range of services began in July 2013 and was completed at the end of 2014. The UHC program diminished the role of insurance companies, as government funds flowed directly to healthcare providers. Renewed hospital infrastructure, combined with the UHC, improved accessibility of care as well as patient satisfaction, with 96.4% of patients satisfied by UHC.
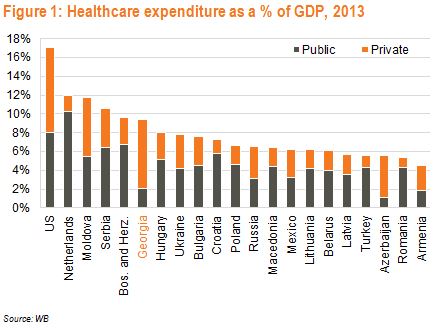
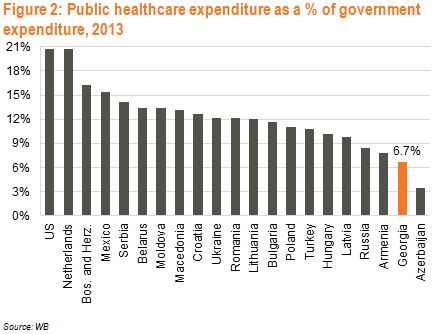
Across the globe, healthcare expenditure models vary, with no single model being systematically and definitively more cost effective. Instead, the application and management of a system determine its efficiency. Many developed, industrialized countries have established healthcare systems with UHC. Under UHC, healthcare is provided by the government (in most cases through private-sector providers) and financed by the government through tax receipts. Depending on the country-specific model, the government controls to a varying degree what operators can charge and defines cost-sharing agreements.
In Georgia, even after the introduction of the current UHC model in 2013, the delivery of care remains reliant on private operators. As a result, Georgia’s UHC model, administered by a state agency (Social Service Agency), is unique: the financing side resembles a pure UHC system, with the government as the program’s major financial contributor and with cost-sharing in the form of co-payments (out-of-pocket) by beneficiaries. The state now negotiates rates with and funds the largely private healthcare providers directly, bypassing insurance companies. Notably, under UHC, healthcare providers shifted to retail business, as beneficiaries became free to choose medical providers.
All in all, several tides of health reforms, backed by strong political support, fostered a competitive environment in the healthcare sector by attracting private companies. The latter made considerable investments in the sector, which, combined with the MoLHSA’s liberalization policy and increased government healthcare spending, create room for sustained growth in Georgia’s healthcare sector.
David Ninikelashvili (Galt and Taggart)